Causes of Dysbiosis
Currently, the scientific community has established four main causes of intestinal dysbiosis:
- Fermentation
- Putrefaction
- Sensitization
- Deficiency
Fermentation
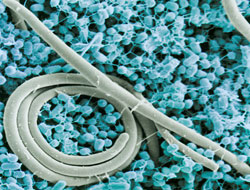
 Fermentation (also known as small bowel bacterial overgrowth) is a condition which causes carbohydrate intolerance due to overgrowth of bacteria located within the stomach, small intestine, and the proximal part of the large intestine.
Fermentation (also known as small bowel bacterial overgrowth) is a condition which causes carbohydrate intolerance due to overgrowth of bacteria located within the stomach, small intestine, and the proximal part of the large intestine.
Bacterial overgrowth can be induced by a number of reasons including:
- Hypochlorhydria – a condition during which the parietal cells of the stomach do not produce the normal amount of hydrochloric acid, which causes the content of the stomach to become more alkaline.
- Dysmotility and stasis of the small and large intestine – cause the content of the gastrointestinal tract to remain immobile for a prolonged amount of time, giving the harmful bacteria the time to multiply.
- Surgical operations – surgical operations on the gastrointestinal tract often cause temporary stasis of its peristaltic movements, which (as mentioned above) is one of the factors that promote the bacterial overgrowth.
- Immune deficiency – it may not seem apparent, but our immune system is at constant war with the bacteria that reside within our gastrointestinal tract, preventing them from multiplying out of control. Due to various conditions, including HIV, immunosuppression therapy, and therapy of autoimmune disorders using glucocorticoids, can lower the ability of the immune system to suppress the constantly multiplying bacteria, which reside in our gastrointestinal tract.
- Malnutrition – is a continuation of the previous point, since malnutrition decreases the body’s ability to resist the harmful bacteria which reside within the gastrointestinal tract.
Bacterial overgrowth increases the likelihood of systemic infections as well as causing carbohydrate intolerance, since any carbohydrate that is being ingested gets fermented by the harmful bacteria, which causes them to release toxic waste products.
Carbohydrate intolerance is often the only symptom of bacterial overgrowth, making it very similar to intestinal candidiasis. In either of those cases, sugars are being fermented to produce ethanol. Overall, carbohydrate intolerance is more likely to be caused by yeast infection (80% of the cases) than by bacteria (20% of the cases). Symptoms of bacterial overgrowth include:
- Abdominal distension – accumulation of gas within the large and small intestine, which creates a feeling of abdominal pressure, fullness, nausea, cramping, and even pain. This gas is released by the bacteria as they ferment the carbohydrates.
- Carbohydrate intolerance – the person is unable to ingest simple and complex carbohydrates, which often leads to fatigue, irritability, and malnutrition.
- Impaired mental function – is caused by both the toxins (endogenous ethanol) released by the bacteria and by the lack of carbohydrates which are the main source of energy for our body and especially the brain.
Some studies link bacterial overgrowth to gastric cancer, as well as to acidosis (blood’s pH becomes more acidic), caused by excessive production of lactic acid.
Putrefaction
 Putrefaction dysbiosis is caused by a diet that is high in meat and fat, while being low in insoluble fibers. Such a diet may lead to a higher concentration of Bacteriodes and lower concentration of Bifidobacteria within the lumen of the large intestine. This causes:
Putrefaction dysbiosis is caused by a diet that is high in meat and fat, while being low in insoluble fibers. Such a diet may lead to a higher concentration of Bacteriodes and lower concentration of Bifidobacteria within the lumen of the large intestine. This causes:
- A higher bacterial urease activity and increased bile flow.
- Increased formation of tumor-promoters as a result of fermentation of bile acids by the bacterial enzymes.
- Decrease in production of short-chain fatty acids due to lower concentration of beneficial bacteria.
- Increase in stool pH, which is primarily caused by a higher ammonia production.
- An increase in deconjugation of excreted estrogens, which enables them to be reabsorbed into the body, raising the levels of plasma estrogen.
Putrefaction dysbiosis can be corrected by lowering the amount of dietary meat and fat, and increasing the consumption of fibers and preparations which contain high concentrations of Lacto- and Bifidobacteria.
In essence, the majority of adverse effects of Putrefaction dysbiosis are caused by an increase in metabolic activity of luminal organisms. These adverse effects include:
- Higher concentrations of Klebsiella, Proteus, and Bacteroides cause the levels of a certain enzyme - urease. This enzyme can hydrolyze urea to form ammonia, which raises the stool pH, which is linked with colon cancer.
- Decarboxylation of amino acids by the altered luminal bacteria creates neurotoxic and vasoactive amines, including tryptamine, tyramine, octapamine, and histamine. Usually the liver deaminates these amines to inactivate them. However, severe cirrhosis can prevent this from happening which can contribute to hypotension and encephalopathy.
- Luminal bacteria also produce bacterial tryptophanase which can degrade tryptophan (an amino acid) to form carcinogenic phenols.
- A bacterial beta-glucuronidase hydrolyzes conjugated estrogens, which disrupts the normal regulation of estrogen levels within the body, as it increases the recirculation of estrogen. A Western diet that is rich in meat can therefore increase the levels of deconjugating enzymes, which increases reabsorption of estrogen and contributes to the development of breast cancer as well as to other adverse effects.
- Beta-glucuronidase, created by bacteria, can also deconjugate bile acids. Such bile acids become toxic to the interior lining of the colon and cause diarrhea. Deconjugated bile acids and their metabolites have cancerogenic effects, which can lead to colon cancer or ulcerative colitis.
- The luminal bacteria also decrease the levels of primary bile acids (cholate and chenodeoxycholate), while increasing the levels of secondary bile acids (deoxycholate and lithocholate). These secondary bile acids are reabsorbed less efficiently and may cause colon cancer. Studies have established a strong link between the concentration of deoxycholate within the stool and the likelihood of colon cancer.
It must be noted that not all metabolic processes of luminal bacteria are harmful. Beneficial bacteria, such as Bifidobacteria, ferment soluble fibers to form short-chain fatty acids (mainly butyrate) which have a nourishing effect on the colonic mucosal cells.
Butyrate, created by beneficial bacteria, is also responsible for:
- Inducing differentiation of neoplastic cells (prevents cancer);
- Decreasing reabsorption of ammonia by the intestine;
- Decreasing inflammation caused by ulcerative colitis;
- Decreasing cholesterol synthesis within the liver;
- Lowering stool pH, which decreases the likelihood of colon cancer.
Sensitization
This type of dysbiosis occurs when the immune system reacts to the normal indigenous intestinal microflora and its components. This condition may lead to various diseases such as spondyloarthropathies, inflammatory bowel disease, and skin disorders such as acne and psoriasis. This condition often complements fermentation dysbiosis and requires similar treatment.
Deficiency
Use or misuse of antibiotics, or a diet that is poor in soluble fiber can cause absolute deficiency of beneficial bacteria, including E. coli, Lactobacillus, and Bifidobacteria. This can be diagnosed directly by identifying the levels of Lactobacillus or E. coli within the stool, or indirectly by measuring the levels of fecal short-chain fatty acids. Putrefaction and deficiency often go hand in hand and have the same treatment.
